As you conduct a standard search for physician assistant trends, including salary, admissions statistics, required prerequisite coursework, program costs, etc. you will come across various weblogs and resources that contain data and statistics to varying degrees. Finding the most up-to-date statistical information and distinguishing what is and isn't relevant can be challenging.
The good news is that the majority of the data you uncover during your search is sourced from only a handful of research articles published on a regular basis by a small subset of reliable sources. Mainly the Physician Assistant Education Association (PAEA) and the National Commission on Certification of Physician Assistants (NCCPA).
This data is usually published online and made available as a series of free PDF downloads. Each research report is packed full of statistical information that (while detailed) can contain significant overlap.
Although both the NCCPA and PAEA have made significant progress in creating more user-friendly reports (including visual aids and graphics), the overlap between these reports and the sheer amount of data can be overwhelming.
In this blog post, I will summarize key findings from the most influential national reports on PAs by organizations from the Physician Assistant Education Association (PAEA), the National Commission on Certification of Physician Assistants (NCCPA), and the American Academy of PAs (AAPA).
Moreover, I aim to create an up-to-date repository of these resources that you can bookmark and revisit as new reports and data are released.
Major topics covered in these reports include:
- Demographics of recently certified and currently practicing PAs
- Specialty preferences and clinical practice settings
- Salaries, incentives, and compensation benchmarks
- PA program tuition, enrollment, and graduation trends
- Student debt and postgraduate pursuits
- Burnout rates and job satisfaction
- And much more...
PAEA Research and Reports
PAEA conducts several annual research initiatives and surveys of member programs, faculty, and students. These reports aim to learn more about the issues facing PA education and the profession, support PA programs and decision-makers with the best data, and empower PA researchers.



1. Program Report (latest #35 October 2020)
PAEA's longest-running research endeavor collects information about program operations, program and student financial information, student and faculty characteristics, and more.
Here are some key findings from the latest PAEA Program Report:
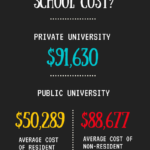
- The average PA program tuition continues to rise, reaching $95,058 for private programs $52,585 (in-state), and $93,313 (out-of-state) for public programs in 2018-2019. This reflects a 3-5% increase from the previous year.
- More PA programs are paying for clinical rotations - in 2019, 52% of programs reported paying for some or all clinical rotations, up from 48% in 2018. The average payment was $291 per student per week.
- The average first-year PA class size was 48 students, continuing an upward trend. Total enrollment across all PA programs was 29,341 students. Graduating class sizes averaged 44 students.
- The student-to-faculty ratio was 13:1 based on full-time faculty headcount or 12:1 based on full-time equivalent (FTE) faculty counts.
- In the 2019 graduating cohort, the on-time graduation rate was 93.5%. The top reasons for delays in graduation or dismissal were academic issues, personal reasons, and deceleration to the next cohort.
2. Faculty and Director Report (latest #4 July 2020)
This report informs the association and PAEA member programs about employment trends that may affect the recruitment and retention of PA faculty and directors.
Here are some key highlights from the latest PAEA Faculty & Directors Report:
- Average faculty salary was $99,771. The average program director's salary was $135,493.
- The top factors faculty considered most important when applying for positions were location, work-life balance, job stability, fringe benefits, and reputation of the institution/program.
- 67.4% of faculty reported working clinically. Of those, average hours of clinical work per week was 11.6 on own time and 8.2 hours on release time.
- 46.9% of faculty had ever published research or scholarly work over their academic careers. In the past 2 years, 30.1% had published.
- 14.0% of faculty had received external funding for research or scholarly work in the past 3 years.
- Top faculty stressors were self-imposed expectations, increased work responsibilities, institutional procedures/red tape, and lack of personal time.
- If given the choice, 76.7% of faculty would probably or definitely still work at their current program, while 82.0% would probably or definitely still be a PA educator.
3. Curriculum Report (latest #6 February 2023)
This survey is administered in three parts that rotate annually and correspond to the major phases of PA school: the prerequisites/admissions phase, the didactic phase, and the clinical phase.
Here are some key highlights from the PAEA curriculum reports on clinical, didactic, and prerequisite curricula:
Clinical Curriculum Report
- Over 90% of programs required ACLS, BCLS, HIPAA, and completion of the didactic phase before students could participate in clinical rotations.
- The average program required 9 distinct rotations, 47 weeks, and 1,752 contact hours of supervised clinical practice experiences (SCPEs).
- Over 70% of programs used Typhon or E*Value to track student contact hours. About 35% used Excel or other spreadsheets to schedule SCPEs.
- Over half of programs were paying for some or all clinical sites due to competition from other PA programs and other health professions students. About 30% had increased or considered increasing tuition to cover clinical payments.
Didactic Curriculum Report
- The organ systems-based approach was the most common instructional model and curriculum delivery method.
- The average program devoted 6% of the didactic curriculum to interprofessional education.
- Over 80% of programs required a master's capstone project, most commonly a scholarly paper.
Prerequisite Curriculum Report
- The most universally required prerequisites were anatomy, physiology, microbiology, biochemistry, statistics, and psychology.
- About half of programs required upper division natural science prerequisites with a C letter grade minimum.
- Over 90% of programs used CASPA and required references, a personal statement, an on-site interview, and a seat deposit.
4. Student Report 5: (latest #5 June 2023)
This survey collects rich data from matriculating and graduating students to learn more about reasons for choosing the profession, satisfaction with programs, future practice plans, and more.
Here are some key highlights from the PAEA student surveys:
Matriculating Student Survey (MSS)
- Over 90% of matriculating students decided to pursue a PA career due to the desire to care for patients, mobility between specialties, and work-life balance.
- The average matriculating student applied to 9 PA programs, received 4 interviews, and 2 acceptance offers.
End of Program Survey (EOPS)
- 85% of graduating students participated in required interprofessional education opportunities during PA school.
- Over 90% of graduating students felt prepared across all PA competencies, especially for patient-centered care and self-assessment/professional development.
- 32.3% of 2,065 EOPS respondents said “Yes” they received grants, scholarships, and/or stipends for their graduate PA education.
- 35% of graduating students had either accepted a job offer or received at least one offer, with over half expecting or receiving salaries between $100K-$110K.
- 20% of graduating students reported personally experiencing some form of discrimination or harassment during PA school.
NCCPA Research and Reports
NCCPA has a robust repository of data on Certified PA demographic and practice characteristics. The information collected in the PA profile is compiled and is used to produce four annual reports regarding PA practice.

1. Statistical Profile of Recently Board Certified PAs (latest report 2022)
PAs who have been certified (for the first time) for six months or less. This report highlights the data collected from this module.
Here are the key findings from the 2022 Statistical Profile of Recently Board Certified Physician Assistants report summarized in bullet points:
- There were a record 11,092 recently certified PAs represented in all 50 states and Washington, D.C., in 2022. This is a 19.4% increase from 2018.
- 75.4% of the 2022 cohort are female. The median age is 27 years old.
- 10.6% of recently certified PAs identify as Black/African American, up from 7.9% in 2018. 9.1% indicate they are Hispanic/Latino/Spanish origin compared to 8.0% in 2018.
- 58.9% have accepted a clinical PA position so far, compared to 46.7% at the same point in 2021. 36.2% were still searching for a position.
- 75.4% of those employed received 2 or more job offers. 64% are earning over $100k salary.
- Top specialties are surgical subspecialties (17.4%), emergency medicine (16.4%), and family medicine (16.2%). 21.2% are in primary care, down from 24.0% in 2018.
- 51.3% accepted jobs in hospital settings. 29.9% took positions in private practice offices.
- Of those still seeking jobs, 44.1% prefer to work in the area where they grew up and 39.8% hope for a hospital setting position.
- 58% without a job desire over $100k minimum salary. Top desired incentives are CME/certification reimbursement and professional development.
- In 2022, 3.1% (vs. 1.9% in 2018) of recently certified PAs indicated they are a National Health Service Corps Scholar or a state or federal loan repayment program participant, which requires practicing in a Health Professional Shortage Area (HPSA) or Medically Underserved Area (MUA).
2. Statistical Profile of Board Certified PAs by Specialty (latest report 2022)
Here is a summary of some of the key findings from the 2022 Statistical Profile of Certified PAs by Specialty report:
- Over 140,000 certified PAs provided responses. The top 5 specialties are family medicine (17.1%), emergency medicine (11.2%), orthopedic surgery (10.7%), primary care (23.1%), and dermatology (4.2%).
- 30.8% of PAs have changed specialties 2 or more times in their careers. Occupational medicine (56.2%) and geriatrics (43.9%) had the highest rates.
- 26.0% of PAs reported an increase in clinical opportunities in the past year. The top specialties were cardiothoracic surgery (34.9%), critical care medicine (33.4%), and emergency medicine (30.3%).
- 36.7% of PAs said their employer is hiring. Critical care medicine (63.5%) and oncology (51.7%) had the highest demand.
- 28.5% of PAs have over $100k in educational debt. Critical care medicine (39.2%) and psychiatry (36.6%) were the highest.
- 83.6% of PAs are satisfied with their current job. Satisfaction was highest in plastics (89.0%) and lowest in emergency medicine (78.3%).
- 32.2% of PAs reported at least 1 symptom of burnout. Emergency medicine had the highest burnout rate at 39.9%.
3. Statistical Profile of Board Certified PAs (latest report 2022)
Here is a summary of key findings from the 2022 Statistical Profile of Board Certified PAs:
- There were 168,318 certified PAs in 2022, a 28.4% increase since 2018. 70.6% are female. The median age remains 38.
- Top specialties are surgical subspecialties (18.6%), family medicine (17.1%), and emergency medicine (11.2%).
- 41.7% of PAs work in hospitals. 37.1% work in private practice offices. 5.6% work in urgent care.
- 40.3% of PAs participate in telemedicine, up from 8.7% in 2018. The top telemedicine functions are follow-up with patients (88.8%) and diagnosing/treating (82.8%).
- 34.7% of clinically active PAs have their own patient panel, with a median of 100 patients. An estimated 10.4 million patients are seen by PAs per week.
- 8.7% plan to leave their clinical PA position in the next year, up from 5.6% in 2018. The top reasons are seeking another PA position (57.1%) and burnout (43.3%).
- 32.2% of PAs report at least one symptom of burnout. This is up slightly from 30.6% in 2021.
- Mean income for PAs has risen to $120,204, an 8.7% increase since 2018.
- 5.4% of PAs completed a postgraduate residency or fellowship program. The top specialties are emergency medicine, general surgery, and internal medicine subspecialties.
4. Specialty Supplement Report on Secondary Specialty (latest report 2022)
Here is a summary of some of the key findings from the 2022 Specialty Supplement Report on Secondary Specialty:
- 64.6% of PAs with cardiothoracic vascular surgery as their primary specialty also have it as their secondary specialty. This is the highest rate among the specialties.
- 50.4% of PAs with emergency medicine as their primary specialty also list it as their secondary specialty.
- Critical care medicine PAs have the highest rate (38.9%) of matching primary and secondary specialties.
- Over 30% of PAs in the specialty areas of occupational medicine, physical medicine/rehabilitation, plastic surgery, and pain medicine have changed specialties 2 or more times.
- The top reason PAs reported having a secondary clinical position across most specialties was to supplement earnings from their primary position.
- Emergency medicine is the most common secondary specialty listed among primary specialties.
- The median hours worked per week in secondary specialties is 10 hours across primary specialties. Mean ranges from 8-13 hours per week.
- Urology PAs that have a secondary specialty reported the highest median (15 hours) and mean (14 hours) hours worked in their secondary position.
Other Important Annual Reports
Of the three additional resources on this list, two produce important annual salary reports (AAPA and Medscape). I have included a link as well to The Association of Postgraduate PA Programs, which provides research articles on postgraduate training for PAs. An honorable mention goes out to the PA History Society, which continues to do excellent work in preserving the physician assistant profession’s history and achievements.
AAPA Salary Report
Here is a summary of some of the key findings from the 2023 AAPA Salary Report:
- In 2022, PAs’ median compensation was $120,000 – a 4.3% increase from $115,000 in 2021!
- The median hourly wage was $65.88, up from $63.08 in 2021.
- Median productivity-based compensation was $180,000, also up from $170,000 in 2021.
- In 2022, PAs again said employers were funding professional development at pre-pandemic levels.
Medscape Physician Assistant Compensation Report 2023

Here is a summary of the key findings from the Medscape PA salary report in bullet point form:
- Average PA compensation increased 4% to $134,000 in 2023, up from $129,000 in 2022. Average base pay also rose from $118,000 to $122,000.
- Nearly two-thirds of PAs received a pay increase in 2023 compared to 2022, but 8% saw their income decrease.
- Only half of PAs feel they are fairly compensated in 2023, down from a high of 74% in 2020.
- Most PAs continue to work in medical offices/clinics (48%) or hospitals (30%), with stable proportions in recent years. Just 7% are self-employed.
- The highest-paid PAs work in surgery/OR ($151K) and emergency/urgent care ($148K). Compensation rose the most for acute care and clinic settings.
- Significant compensation gains often go to veteran PAs - those with 21+ years of experience saw 7% pay increases on average.
- Regional pay differences persist - Pacific states tend to pay PAs the most, but the cost of living is also higher.
- Factors beyond salary impact job satisfaction, like work/life balance, respect, and autonomy. Locum tenens provides flexibility.
APPAP
The Association of Postgraduate Physician Assistants Programs website provides a collection of research articles focused on postgraduate training for Physician Assistants and Nurse Practitioners, covering topics like accreditation, selection criteria, and implicit bias training in residency and fellowship programs. It serves as a valuable resource for insights into the latest trends and challenges in PA and NP postgraduate education.
I hope this summary of important data and research serves as a useful overview of the current state of the PA profession in terms of education and practice. The comprehensive information contained in these reports reflects a commitment to using evidence-based policies and planning to support the PA workforce, enabling us to maintain and improve access to outstanding medical care.
If you know of any additional resources or reports that you find helpful, please share them in the comments section. Be sure to bookmark this page for future reference, as we will update it regularly.














Leave a Reply